Niranjan Khadka, Irene E. Harmsen, Andres M. Lozano, Marom Bikson. Bio-Heat Model of Kilohertz-Frequency Deep Brain Stimulation Increases Brain Tissue Temperature. Neuromodulation 2020. DOI: 10.1111/ner.13120
Download PDF published in Neuromodulation — DOI
Abstract
Objectives
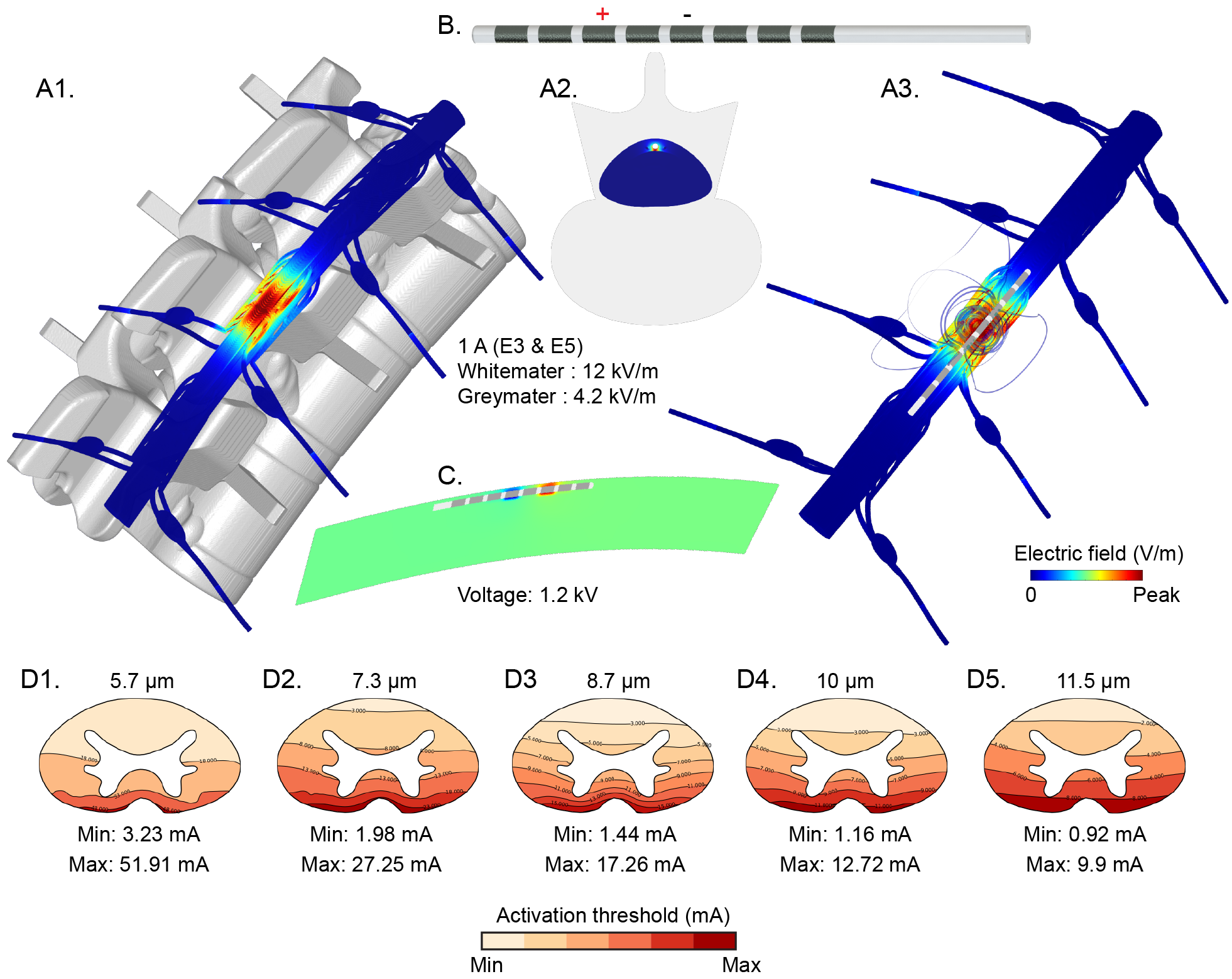
Early clinical trials suggest that deep brain stimulation at kilohertz frequencies (10 kHz‐DBS) may be effective in improving motor symptoms in patients with movement disorders. The 10 kHz‐DBS can deliver significantly more power in tissue compared to conventional frequency DBS, reflecting increased pulse compression (duty cycle). We hypothesize that 10 kHz‐DBS modulates neuronal function through moderate local tissue heating, analogous to kilohertz spinal cord stimulation (10 kHz‐SCS). To establish the role of tissue heating in 10 kHz‐DBS (30 μs, 10 kHz, at intensities of 3‐7 mApeak), a decisive first step is to characterize the range of temperature changes during clinical kHz‐DBS protocols.
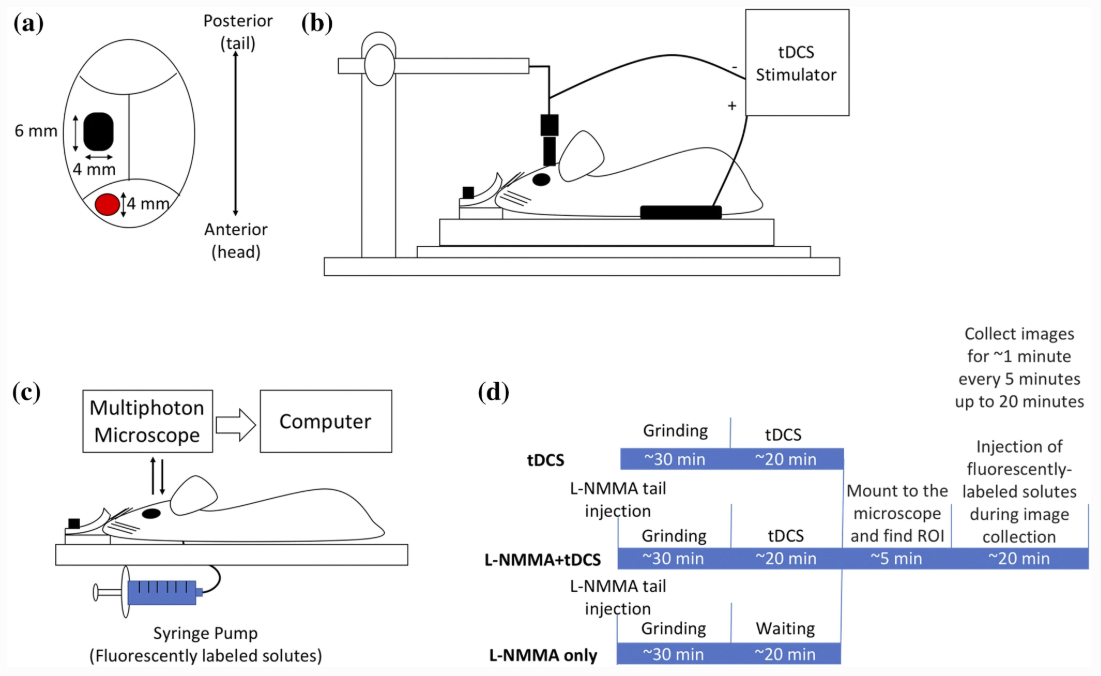
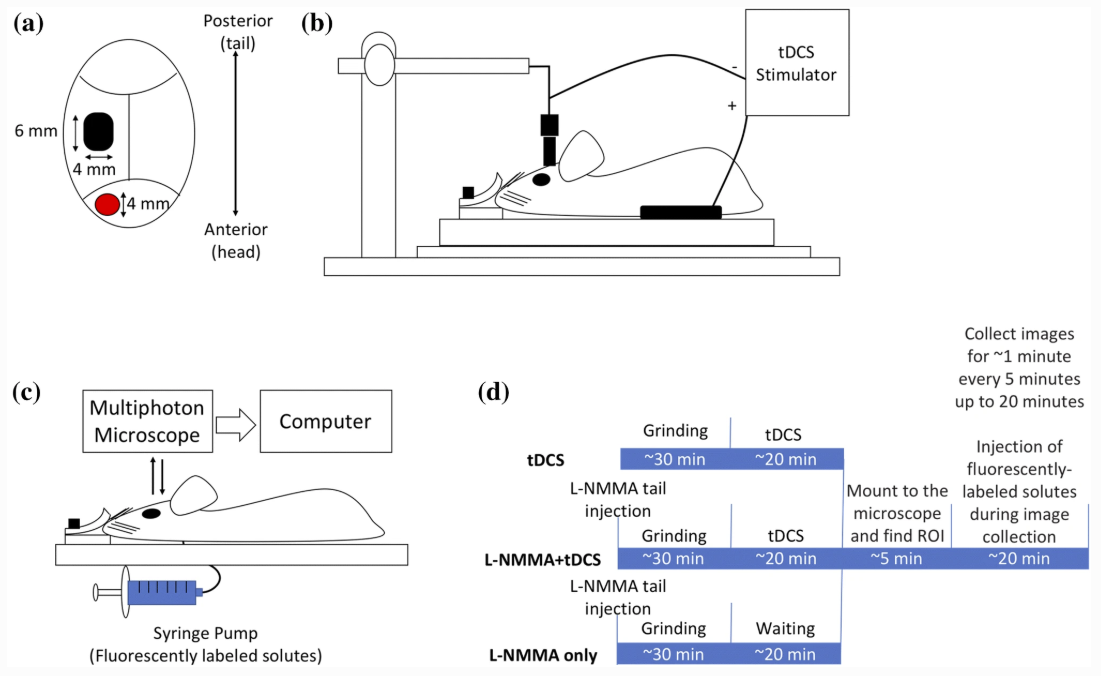
Materials and Methods
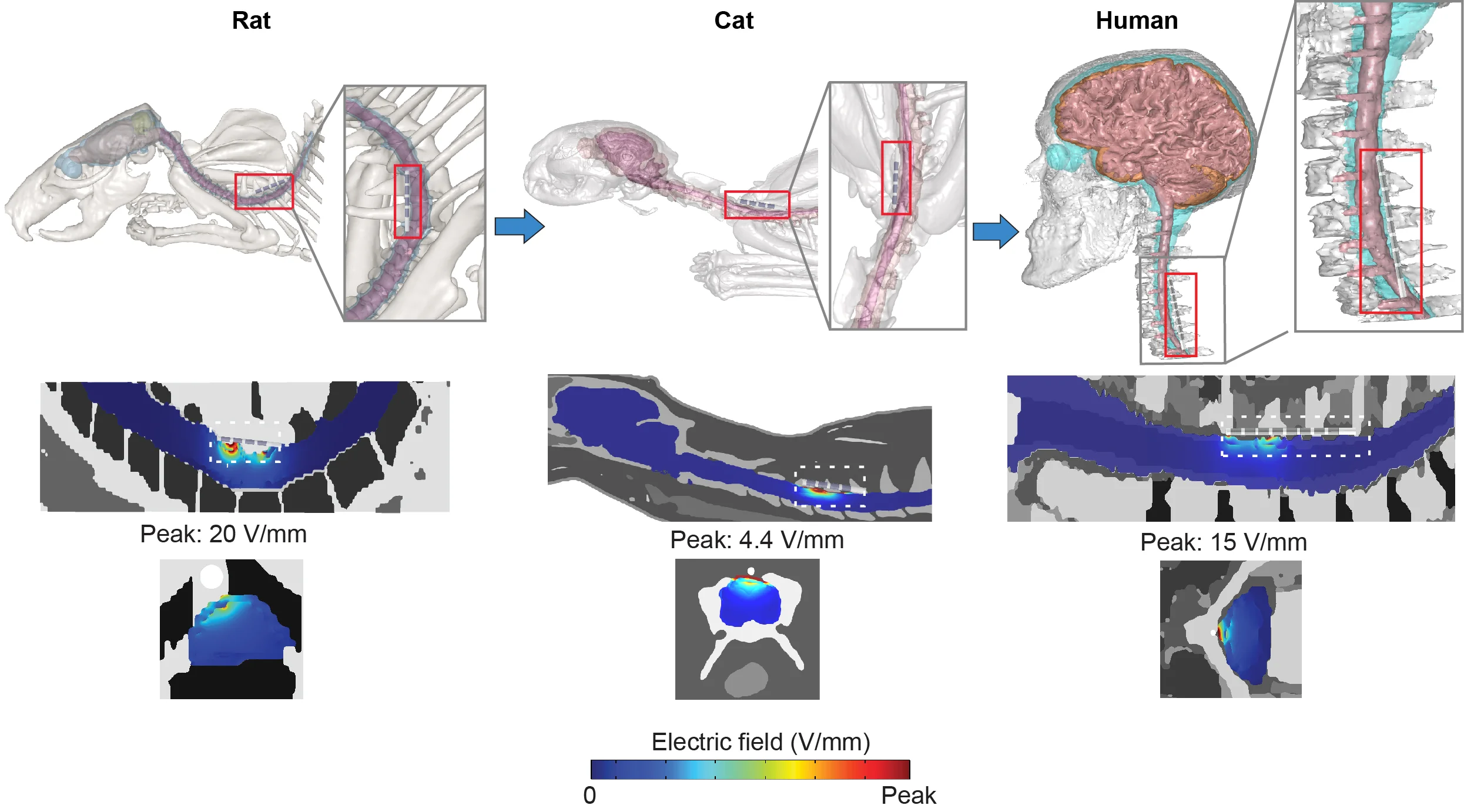
We developed a high‐resolution magnetic resonance imaging‐derived DBS model incorporating joule‐heat coupled bio‐heat multi‐physics to establish the role of tissue heating. Volume of tissue activated (VTA) under assumptions of activating function (for 130 Hz) or heating (for 10 kHz) based neuromodulation are contrasted.
Results
DBS waveform power (waveform RMS) determined joule heating at the deep brain tissues. Peak heating was supralinearly dependent on stimulation RMS. The 10 kHz‐DBS stimulation with 2.3 to 5.4 mARMS (corresponding to 3 to 7 mApeak) produced 0.10 to 1.38°C heating at the subthalamic nucleus (STN) target under standard tissue parameters. Maximum temperature increases were predicted inside the electrode encapsulation layer (enCAP) with 2.3 to 5.4 mARMS producing 0.13 to 1.87°C under standard tissue parameters. Tissue parameter analysis predicted STN heating was especially sensitive (ranging from 0.44 to 1.35°C at 3.8 mARMS) to decreasing enCAP electrical conductivity and decreasing STN thermal conductivity.
Conclusions
Subject to validation with in vivo measurements, neuromodulation through a heating mechanism of action by 10 kHz‐DBS can indicate novel therapeutic pathways and strategies for dose optimization.